Background:
Incidentally discovered thrombocytopenia in asymptomatic individuals often result in a referral to hematology. Clinical decisions for these individuals are mostly based on local practice, as little evidence exists on their risk of hematologic disease and death. We aim to lay ground for an evidence-based clinical approach to incidental thrombocytopenia with or without concurrent anemia by studying relative and absolute risk of being diagnosed with hematologic disease, death from hematologic disease and death from any cause.
Methods:
We studied 382,424 general population individuals from the United Kingdom (UK) Biobank aged 40-70 years, of whom 9,151 had thrombocytopenia with or without anemia. Individuals with leukocytosis, neutropenia or prior hematologic disease were excluded. As a validation cohort, we studied 104,358 Danish general population individuals. All individuals attended a health examination and had platelets, hemoglobin, leukocyte and differential count measured at study enrolment. Individuals were followed prospectively for up to 16 years for hematologic disease and cause-specific death using national registries, covering all deaths and almost all cancer cases in the UK and Denmark.
Results:
Among 382,424 individuals from the UK, 6,044 had hematologic disease during follow-up, 28,403 died from any cause and 1,213 died due to hematologic disease. For all analyses, the reference group was individuals with normal platelet count and normal hemoglobin.
Individuals with isolated mild thrombocytopenia (platelets 100-149 x 10 9/L) or isolated moderate-severe thrombocytopenia (<100 x 10 9/L) had increased relative risk of hematologic disease (multivariable adjusted Cox regression hazard ratios [HR] 2.19; 95% CI:1.94-2.47 and HR 7.68; 6.35-9.29, respectively), death from hematologic disease (HR 1.81; 1.37-2.38 and HR 2.80; 1.45-5.39, respectively) and death from any cause (HR 1.30; 1.22-1.39 and HR 1.84; 1.58-2.16, respectively). Individuals with mild thrombocytopenia combined with mild anemia (hemoglobin 11-11.8 g/dL for women; 11.9-13.4 for men) also had increased risk of hematologic disease (HR 5.36; 3.82-7.52), death from hematologic disease (4.99; 2.49-10.04), and death from any cause (2.57; 2.14-3.10). Relative risk estimates were increased to a similar or higher extent in individuals having moderate-severe thrombocytopenia with mild anemia, mild thrombocytopenia with severe anemia (hemoglobin <11 g/dL for women; <11.9 for men) or moderate-severe thrombocytopenia with severe anemia.
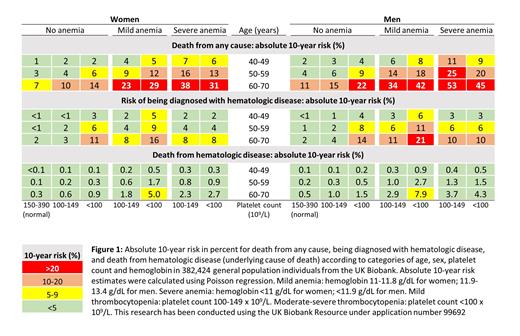
When studying absolute risk (Figure 1), the 10-year risk of death from any cause was especially high (23-53%) in individuals aged 60-70 years with combined thrombocytopenia and anemia. However, 10-year risk of death from hematologic disease was below 5% for all combinations of sex, age, platelet count and hemoglobin, except for women (5.0%) and men (7.9%) aged 60-70 years having moderate-severe thrombocytopenia with mild anemia. For risk of hematologic disease, absolute 10-year risk was below 5% for all age and sex-groups with isolated mild thrombocytopenia, while 10-year risk was as high as 21% in 60-70 year-old men having mild anemia combined with moderate-severe thrombocytopenia.
For individuals with thrombocytopenia with or without anemia, the most common hematologic diseases were lymphoid malignancies (41% of diagnoses; HR 1.73; 1.49-2.01), ITP (34%; HR 22.85; 18.56-28.13), and myeloid malignancies (25%; HR 2.90; 2.39-3.52). Among causes of death in individuals with thrombocytopenia were non-hematologic cancer (35% of deaths; HR 1.21; 1.10-1.33), heart disease (21%; HR 1.43; 1.27-1.62), infections (4%; HR 1.84; 1.36-2.49), and bleeding (2%; HR 1.37; 0.94-1.99).
In the independent Danish validation cohort, results were generally similar to those presented in Figure 1.
Conclusion:
Individuals with thrombocytopenia with or without anemia had increased relative risk of hematologic disease, death from hematologic disease and death from any cause. However, 10-year absolute risk of death from hematologic disease was below 5% for most combinations of sex, age, platelet count and hemoglobin. Our absolute 10-year risk estimates can help clinicians to identify low and high-risk individuals and guide decisions on which individuals with incidentally discovered thrombocytopenia that should undergo investigations for possible hematologic disease.
Disclosures
Glenthoej:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novo Nordisk: Consultancy, Membership on an entity's Board of Directors or advisory committees; Pharmacosmos: Consultancy, Membership on an entity's Board of Directors or advisory committees; Sanofi: Research Funding; Saniona: Research Funding; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; bluebird bio: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bristol Myers Squibb: Consultancy, Membership on an entity's Board of Directors or advisory committees.